The Midwifery Group - Team 3

Laura Willihnganz, Rachel Rees, Jill Freeman, and Kathryn Ward
What are the challenges you’re facing as a midwife practicing during the pandemic?
Rachel: Learning to live underneath PPE is challenging in a personal way: long hours wearing a mask and the subsequent dehydration, feeling light-headed, getting sore ears and chafing on my face; long hours wearing goggles on top of glasses and therefore not seeing as well as I need to, not to mention the fogging glasses from mask-wearing. Professionally the PPE puts distance between myself and my clients. I am used to body language, facial expressions, and breathing together to support people in labour. Adapting to a new schedule of fewer prenatal visits than usual has been challenging for us - it means less contact with each clients, less ability to form relationships or even meet clients before their birth. We really see the value in continuity of care! Additionally it is challenging in general to be a front-line worker in this pandemic. It is a scary time and stress is very high. In the first few weeks I did not sleep through the night (and not just in the usual way for a midwife!). We are working harder than ever and also fear getting the virus ourselves or bringing it home to our families. The stress is deeply exhausting on top of a job that is baseline exhausting.
Laura: I miss having as many in-person appointments with our clients. That deeper connection and relationship building is part of what is so special about midwifery care—both for the client and the midwife—and it's just different over the phone. The increased workload is also challenging. We are still doing the same work, it just takes so much longer with the infection control measures for every client contact, time spent staying up to date on every changing protocols and guidelines, and so much more laundry at home for all the scrubs, clothes and scrub caps we're going through! It's harder to find time for self care (and just doing the basics like groceries and cooking!) with less down time outside of scheduled work hours, at time when ensuring our resilience and health is more important than ever.
How has your midwifery practice changed since the pandemic?
Rachel: Immensely! Here are just a few examples of structural changes:
- We have adapted our prenatal visit schedule to reduce the number of client visits in line with the pandemic recommendations from Perinatal Services BC. This new schedule meets the minimum requirements for antenatal care while maintaining safe practice and healthy outcomes. As noted above, it does reduce our ability to have continuity of care, thus reducing satisfaction for both clients and midwives.
- Our in-person prenatal visits are now shortened to 15 minutes from 30-45 minutes to reduce contacts and keep our waiting room clear. We see people briefly for their physical check-ups and then send them on their way, completing the rest of the usual 30-45 minutes by phone. Clients attend their visits on their own, no partners or support people are allowed. Partners are hearing their babies' heartbeats for the first time by speakerphone.
- We have repacked our home birth gear and on-call equipment from well-organized medical bags into plastic tubs with everything stored in plastic zipper bags. This allows us to keep everything clean and categorized and only need to clean the things we use after a home birth or home visit. The plastic bags and tubs are wiped down after leaving each client's home. While infection control is always a priority and all equipment is cleaned after any home birth, the storage system is a new learning curve. It's tricky to appease my hyper-organized brain that wants my gear stored in logical systematic ways, rather than a box of plastic bags.
- Taking on extra days being on-call for our hospital department colleagues, and while call-outs are paid, the extra on call part is unpaid.
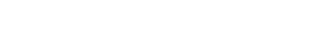
Laura: We can no longer have the relaxed, intimate postpartum home visits we used to—we do physical checks and breastfeeding support efficiently to minimize the amount of time spent in close proximity. I miss perching on the edge of a client's bed and doing a newborn exam with the baby in my lap. I miss involving the older kids in belly checks and showing them how to listen to their new sibling's heartbeat. The basics are all still there, and we're providing excellent safe care, but the many extra things that add warmth and connection aren't as possible these days.
Can you please describe a snapshot of a recent workday?
Rachel: This was a recent Saturday. It started around 9am (luckily I slept through the night; no overnight births that day) with two phone appointments with postpartum clients. It has been a learning curve to consider how to provide breastfeeding support over the phone! I checked our voicemail service and returned clients phone calls. I got dressed in our new home visit uniform: hospital scrubs and a bandana to cover my hair as we did not yet have scrubs caps for community work. Next up was two home visits for post partum clients each with one-week old babies. Each visit required wearing mask, googles, and gloves. After each visit I cleaned all my equipment used in the visit on the sidewalk before putting it back in my car. I thought I might get a chance for some lunch at that point but was paged to see a third trimester client urgently at the hospital - another set of PPE and scrubs used. Between the visits, I returned more incoming client phone calls with questions or health concerns. I got a short break to go home to eat and work on processing the incoming lab results for the day. Before long, I was paged again to attend a home birth as the second backup midwife. Back into my third set of scrubs for the day, and I was off to support another local midwife in welcoming a sweet new baby. It was a hot sunny late afternoon and the sun was streaming in the windows of their small apartment, which meant the sweat was streaming down my body underneath my PPE. One more round of returning client calls ended my work day by 7pm, though I was still on call another 24 hours and more fun was to come...
Kathryn:
0010 Page for active labour. Up out of bed, into scrubs because I’m anticipating this is going to go quick.
0020 Out the door with a set of clothes to change into after the delivery in a Ziploc bag and some snacks. Phone call to the hospital to inform them I’m heading in.
0025 Page back by client requesting I attend her at home because she doesn’t think she’ll make it to the hospital while she waits for childcare for her toddler (only one support person allowed in hospital!).
0026 Call to my second midwife and ask them to bring some medications and additional PPE.
0040 Arrive to clients house, quickly throw on a mask, eye protection and gloves as I come through the door and have a beautiful delivery. Second midwife also arrives right on time!
0350 Transfer to the hospital for some postpartum monitoring by ambulance. Mom and babe both stable! Home birth equipment wiped down and packed by my amazing back-up into my car. Paramedics, in their new gear, do an incredible of being respectful of family and transporting us with ease.
0400 Arrive to hospital. Fresh set of scrubs and mask after doffing my gloves and sanitizing at the door. Paged by another client in labour!
0500 Say goodbye to client #1, head to assess client #2 who has just arrived.
0800 Able to go remove my mask, splash some water on my face, and get a cup of some much needed coffee.
0830 Back into the room in a fresh set of scrubs and mask. Eye protection wiped down!
1130 Delivery of Baby #2 in full PPE.
1300 Over to the postpartum ward to see client #1. Sanitizing my hands after looking at the client’s chart and after opening the door.
1330 Back to see client #2 and sign discharge orders because they are ready to go home!
1430 Call an Uber because my car isn’t at the hospital…
1445 Into a fresh set of scrubs (because I didn’t bring other clothes with me in the ambulance) and into an Uber Tesla. A very considerate human who helped show my tired brain how the door handles on a Tesla work.
1455 Arrive back to my car and sanitize my hands before getting in and make my way home.
1510 Back home to doff clothing and personal items appropriately, washing my hands and showering! My keys, phone and pens go into a bin that I wipe down safely. Check messages, make some phone-calls, check labs.
1600 NAP TIME!
1800 Handover to on-coming RM to debrief the last 18hours…
Laura: Last Friday I came on call to two people in early labour. One paged shortly after in rocking labour and we went rushing into the hospital. We had such great support from the nurses and anesthesiologist as we rushed to get her settled and the pain relief she wanted before her baby came! While all this was going on, I was fielding pages from a midwife who needed help for a client of hers while she was supporting someone else in labour at a different call—and a postpartum client who was having a late hemorrhage at home and needed to come in for care. In and out of PPE for each person, and up and down more flights of stairs than I can count between the birthing suites and assessment room! Just after the first sweet baby was born, our awesome obstetrical colleagues updated me that the second client's induction was moving forward quickly now and soon another parent was cuddling their brand new babe. 12 hours after I ran out of the house, I was back home in my little "hot zone" inside the front door where I take off the clothes I'd been wearing and put them in a bucket for washing later, disinfect my keys and pager, etc., shower off and crawl into bed. I had 4 lovely hours of sleep before starting in on what would be a 13 hour day, full of home visits for the other team (our new guidelines to reduce traffic coming and going from the hospital is that one team does all the visits while the other does the ones in the community) and hand washing and donning and doffing and charting and fielding pages for miscarriages and postpartum issues and reviewing labs. I must have eaten sometime in there?!? The things that stand out from that wild shift are the incredible collaboration that makes such a difference, and that while so much has changed in our lives recently, birth is still birth in all it's beauty and intensity.
What, if anything, is helping you get through this crisis?
Rachel:
- My incredible colleagues who are all working so hard to support each other as we learn how to integrate rapidly changing new information into our practice.
- Exercise when I have the energy for it.
- Long baths and meditation when I need rest.
Kathryn:
- Connecting with colleagues and family (via phone, video chat, across the room chats!) to remind me we truly are all in this together.
Laura: Community on all scales—from the incredible teamwork within our clinic and our city-wide Midwifery Department, to the clients asking how we are holding up and being gracious about the changes, to the friends and strangers sewing and 3D printing us PPE to use when there isn't enough through the healthcare system, to the city cheering for all front line workers at 7pm. It makes such a huge difference to be recognized for the essential work that we do, and know that we're making a difference in a meaningful way. And lots of meditation, chocolate and running in the woods at weird times.
Is there anything else you’d like to add?
Laura: I hope that the huge and essential contribution that midwives are making in our communities is seen and remembered by the health care system moving forwards, and midwives are better recognized for the vital role we have in maternity care. And I truly hope that the amazing teamwork and genuine care for those around us are holding up is something that lasts beyond this pandemic.