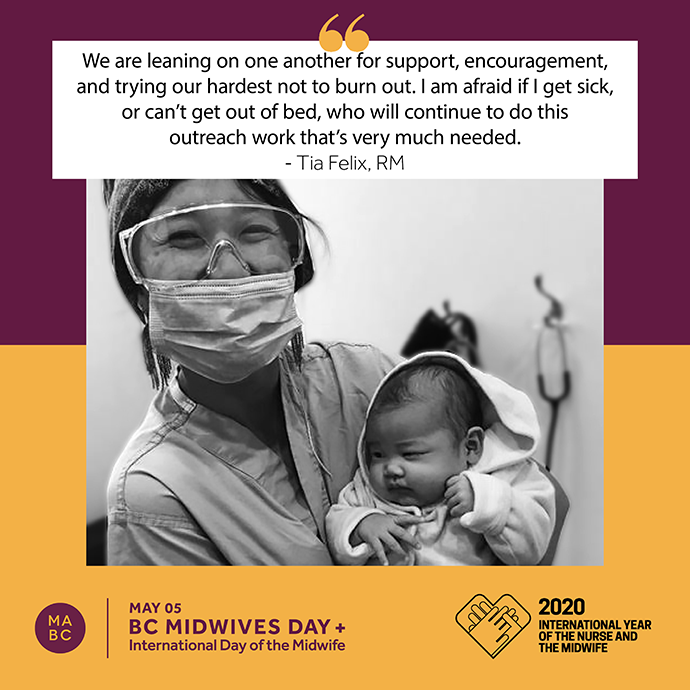
Tia Felix
What are the challenges you’re facing as a midwife practicing during the pandemic?
I primarily work as an outreach Indigenous midwife offering culturally safe, harm reducing and trauma informed model of care to vulnerable populations throughout Vancouver and the surrounding area. Some common challenges include lack of communication (no minutes/wifi), limited transportation and home visits. For example, if my client is unable to come into clinic, or unable to either call or text, I typically offer a home visit. I also routinely reach out to cultural supports such as our wonderful elders and doulas. We miss our elders warmth, wisdom and meals that they share with our families. Our Indigenous doulas are limited to accompany families to the hospital. We had paused our prenatal/postnatal classes which has left many families who either lack wifi or funds, we are doing a lot of teachings over multitude forms of communication. Community resources that provide food, clothing and various donations are limiting services.
How has your midwifery practice changed since the pandemic?
Since the pandemic, it has highlighted gaps in care and how midwifery can help by providing continuous, accessible, and supportive care for expecting families. However, increasing the demand and workload of midwives. We are continuing to change and adapt to the community recommendations, including working 24 hours 7 days a week. We are leaning on one another for support, encouragement and trying our hardest not to burn out. I am afraid if I get sick, or can’t get out of bed, who will continue to do this outreach work that’s very much needed. We as care midwives, we do not get increase in pay, paid sick leave and or scheduled breaks. Everyday, I feel that I am reducing ways to prevent the spread of COVID-19, limiting traffic to the hospital, early discharges, offering home birth as a way to keep expecting families safe.
Clinically, we are limiting in-person visits, taking multitudes of precautionary measures like wiping anything and everything, gown and gear alterations, and routinely screening for symptoms. As before, offering choice of birth place, including home. Our families and staff continue to understand the ongoing changes, they have provided PPE such as masks and caps. We’ve received words of encouragement and meals to keep us fed to continue working. We also moved locations in the middle of a pandemic, which I don’t recommend.
Can you please describe a snapshot of a recent workday?
A snapshot of my day includes gowning up for home visits, swapping clothes for hospital visits, while answering pages from other families, healthcare workers or others including social workers, mentors, and resource workers. I provide clinic at four different sites throughout the week while still on call. I try to sneak a snack somewhere and meals when offered.
What, if anything, is helping you get through this crisis?
I am from the Interior and a lot of my family, friends and elders are there. They check up on me to see how I am holding up, some days it's tears, others are dry humour laughs. Finding hobbies together. Taking a breather in the garden and most recently, my partner has gotten into sourdough.
Is there anything else you’d like to add?
I want to thank everyone for stepping up and providing all the supports they can! I see and hear you, including the 19:00 PM saxophone player. Kukwstsamc!